| Case report | Peer reviewed |
Cite as: Headley SA, Silva LC, Okano W. Cerebral abscesses in a pig: Atypical manifestations of Streptococcus suis serotype 2-induced meningoencephalitis. J Swine Health Prod. 2012;20(4):179–183.
Also available as a PDF.
SummaryThis article describes the findings associated with Streptococcus suis serotype 2 in a 2.5-month-old mixed-breed male pig. Clinically, the animal demonstrated torticollis, paddling movement, lateral recumbency, and convulsions. Gross evaluation of the brain revealed multiple abscesses, asymmetrically located within the right cerebral hemisphere and in contact with the meningeal surface. Histopathological evaluation revealed multifocal to coalescing cerebral abscesses associated with intralesional bacterial colonies and purulent meningoencephalitis with vasculitis. Biochemical analysis demonstrated that the intralesional bacterium was a gram-positive coccus, with negative reactions to the Voges-Proskauer, catalase, and NaCl assays, and produced acid in trehalose and salicin broths. A polymerase chain reaction assay, using DNA from bacteria cultured from the brain abscesses, amplified the partial 459 base-pair fragment of the capsular gene of S suis serotype 2. The histopathological, microbiological, and molecular findings support a diagnosis of S suis serotype 2-induced cerebral abscesses with meningitis. This case represents an atypical manifestation of streptococcal meningoencephalitis of swine and is, to our knowledge, the first description of S suis serotype 2-induced cerebral abscesses in pigs. | ResumenEste artículo describe los hallazgos asociados con Streptococcus suis serotipo 2 en un cerdo macho de raza mixta de 2.5 meses de edad. Clínicamente, el animal mostraba tortícolis, movimiento de pataleo, recumbencia lateral, y convulsiones. La evaluación macroscópica del cerebro reveló múltiples abscesos, ubicados asimétricamente dentro del hemisferio cerebral derecho y en contacto con la superficie de la meninge. La evaluación histopatológica reveló abscesos multifocales adheridos a colonias bacterianas intralesionales y meningoencefalítis purulenta con vasculitis. El análisis bioquímico demostró que la bacteria intralesional era un coco gram-positivo, con reacciones negativas a las pruebas de Voges-Proskauer, catalasa, y NaCl, y que producía ácido en caldos de trehalosa y salicina. Una prueba de reacción en cadena de la polimerasa, utilizando DNA de cultivo de bacteria de los abscesos del cerebro, amplificó el fragmento parcial de 459 pares de bases del gene capsular del S suis serotipo 2. Los hallazgos moleculares, microbiológicos, e histopatológicos sustentan un diagnóstico de absceso cerebral con meningitis inducido por S suis serotipo 2. Este caso representa una manifestación atípica de meningoencefalítis estreptococal de cerdo y es, a nuestro conocimiento, la primera descripción de abscesos cerebrales inducidos por S suis serotipo 2 en cerdos. | ResuméLe présent article rapporte les trouvailles associées à une infection par Streptococcus suis sérotype 2 chez un porcelet mâle âgé de 2.5 mois. Cliniquement, l’animal présentait un torticolis, des mouvements de pédalage, un décubitus latéral, et des convulsions. Une évaluation macroscopique du cerveau a révélé la présence de nombreux abcès, disposés de manière asymétrique dans l’hémisphère cérébral droit et en contact avec les méninges. L’examen histopathologique a permis d’observer des abcès multifocaux et coalescents associés à des colonies bactériennes intra-lésionnelles ainsi qu’une méningoencéphalite purulente avec vasculite. Les analyses biochimiques ont démontré que les bactéries intra-lésionnelles étaient des coques à gram positif, avec des réactions négatives pour les tests de Voges-Prauskauer, la présence de catalase, et la tolérance au NaCl, et produisaient de l’acide dans des bouillons contenant du tréhalose et de la salicine. Une réaction d’amplification en chaîne par la polymérase, utilisant l’ADN des bactéries obtenues des abcès cérébraux, amplifia le fragment partiel de 459 paires de bases du gène de la capsule de S suis sérotype 2. Les trouvailles histopathologiques, microbiologiques, et moléculaires appuient le diagnostic d’abcès cérébraux et de méningite causés par S suis sérotype 2. Ce cas présente une manifestation atypique de méningoencéphalite à streptocoque porcine et est, selon nous, la première fois que des abcès cérébraux associés à S suis sérotype 2 sont rapportés chez le porc. |
Keywords: swine, Streptococcus suis serotype 2, neuropathology, bacteriology, polymerase chain reaction, PCR
Search the AASV web site
for pages with similar keywords.
Received: December 21, 2011
Accepted: April 12, 2012
Streptococcus suis is an important gram-positive bacterial pathogen of swine that occurs worldwide and is frequently associated with encephalitis, meningitis, arthritis, septicemic processes, endocarditis,1-3 bronchopneumonia, polyserositis, rhinitis, pericarditis,1,2 and abscesses.2 Although the number of serotypes of S suis has reached 35,4 serotype 2 is the most virulent and most frequently isolated in diseased animals.5 Epidemiological studies in southern and southeastern Brazil have suggested that infections in clinically affected pigs are predominantly associated with S suis serotype 2.6-8
Although pigs are more commonly infected by S suis, disease has been infrequently diagnosed in ruminants and horses2,3 and in cats, dogs, and deer.2 Additionally, S suis is a zoonotic disease,9,10 with most cases of human infections occurring in Europe and Asia.9 Streptococcus suis is frequently isolated in pigs submitted for slaughter with manifestations of valvular endocarditis11,12 or meningitis13,14 or with cardiac-associated brain lesions.15 Nevertheless, meningitis is the most important clinical manifestation of porcine S suis infection.9 However, descriptions of S suis-induced cerebral abscesses were not located in major databases. In swine, abscesses have been frequently associated with Streptococcus porcinus in what are commonly known as jowl abscesses, streptococcal lymphadenitis, cervical abscesses,3,10 feeder boils, or swine strangles,16 but these are cutaneous or subcutaneous lesions affecting lymph nodes without involvement of the central nervous system.
A tentative diagnosis of S suis is easily obtained in diseased pigs and is based on characteristic clinical manifestations, the age of the infected animal, and gross pathology.5,10 Confirmation of infection in pigs requires bacterial isolation and observation of histopathological alterations in affected tissues.5,9 Routine identification of S suis is generally based on the following criteria: absence of growth in 6.5% NaCl agar, a negative reaction to the Voges-Proskauer (VP) test, and acid production in trehalose and salicin broths.1,3 Further characterization of S suis has been achieved by polymerase chain reaction (PCR) assay that targets the capsular gene of S suis serotype 2.17,18 This report describes the findings associated with S suis serotype 2-induced cerebral abscesses in a pig and extends the spectrum of disease syndromes associated with this pathogen.
Case description
Clinical history
Three 2.5-month-old mixed-breed pigs (two males and one female) that were maintained on a small subsistence farm located within the city of Arapongas, Paraná, southern Brazil, reportedly demonstrated manifestations of neurological dysfunction, including paddling, incoordination, and inability to stand. Two of the affected pigs died within 3 days after neurological manifestations were observed; the other male pig was submitted to the Veterinary Teaching Hospital, Universidade Norte do Paraná (VTH-UNOPAR), Arapongas, Paraná, Brazil, for evaluation and treatment in late September 2011. On arrival, the animal was very thin, but did not demonstrate clinical manifestations of disease during 2 days of observation and was thus discharged without being subjected to therapeutic intervention. However, when the pig was returned to the farm, similar neurological manifestations were reportedly observed by the owner, who indicated that these became more intense, progressive, and regular. The pig was readmitted to the VTH-UNOPAR 7 days later in extremis, demonstrating torticollis, paddling movement, lateral recumbency, and convulsions. The owner requested euthanasia. The duration of the period between the reported onset of neurological manifestations and necropsy was 21 days. The attending veterinarian indicated that there was no history of reproductive or respiratory disease in the herd and that the ration was composed of commercially produced corn admixed with household waste. Additionally, it is uncertain if the pig had been medicated at the farm. Further, the additional nine weaned pigs, one boar, and three sows at the farm did not demonstrate similar clinical manifestations. Initial differential diagnoses included streptococcal meningitis and porcine herpesvirus.
A routine necropsy was performed soon after euthanasia. Selected tissue (lungs, liver, kidneys, intestine, and lymph nodes) and brain (from several areas) were collected, fixed by immersion in 10% buffered formalin solution, and routinely processed for histopathological evaluation. Duplicate tissue sections of the brain were stained by the Masson’s trichrome, periodic acid-Schiff (PAS), and Grocott methenamine silver (GMS) stain techniques. Swabs of brain abscesses and fresh brain sections that included abscesses were collected for bacteriological analyses. Aliquots of the cultured bacteria derived from the brain were submitted for PCR testing at the Veterinary Microbiology Diagnostic Laboratory, Universidade Federal de Mato Grosso (UFMS), Cuiabá, MT, Brazil. The PCR protocol used was specific for S suis serotype 218 and consisted of the primer pairs (cps2J-s and cps2J) that were designed to amplify the 459 base pairs (bp) of the capsular gene (cps) of this bacterium.17
Gross findings
A routine necropsy at the Laboratory of Veterinary Pathology-UNOPAR revealed lesions close to the right inner ear, restricted primarily to the brain. There was a 3.5-cm diameter, firm, slightly raised, light-green mass centrally located at the right cerebral hemisphere (Figure 1). The meningeal vessels were discretely congested and the cerebral sulci were shallow with distended gyri. Transverse sections of the formalin-fixed brain revealed several abscesses, varying from 0.3 to 0.7 cm in diameter, asymmetrically located throughout the right cerebral hemisphere. The brain stem and cerebellum were not affected. These multifocal to coalescing space-occupying abscesses resulted in marked destruction of the white and gray matter of the right cerebral hemisphere and moderate dilation of the contralateral ventricle (Figure 2). The margins of some abscesses were externally delimited by the meningeal surface, and some abscesses were contiguous with the lateral ventricle. Endocarditis and arthritis were not observed, and no other organs or systems were affected.
Figure 1: Gross demonstration of cerebral abscess in the brain of a 2.5-month-old mixed-breed pig. A large firm mass, 3.5 cm in diameter, is evident in the right cerebral hemisphere (arrow). Scale in centimetres.  |
Figure 2: Formalin-fixed section of the brain of a 2.5-month-old mixed-breed pig. Within the right cerebral hemisphere, there are several inspissated green abscesses (arrows) of varying sizes (0.3 to 0.7 cm in diameter). Observe that some abscesses are externally located at the meningeal surface while others are in contact with the lateral ventricle. Note also that the left lateral ventricle (star) is dilated. Scale in centimetres. 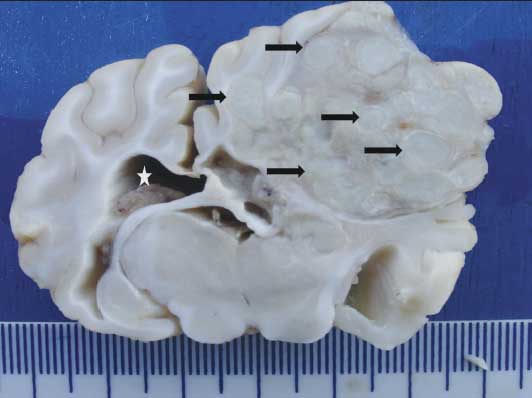 |
Histopathological alterations
Significant histopathological alterations were restricted to the cerebrum; no other systems or tissues were affected. Neurological lesions were characterized by multifocal to coalescing abscesses that were located throughout the cerebrum. Some abscesses were adjacent to the meningeal surface and others were deep within the neuroparenchymal tissue or in contact with the ependymal layer of the cerebral ventricle (Figure 3). Few abscesses contained intralesional bacterial colonies. In most tissue sections, the abscesses were surrounded by varying amounts of connective tissue, this being more evident in abscesses that were contiguous with the meningeal surface. Masson’s trichrome stain clearly identified the extensive connective tissue that encapsulated the abscesses (not shown). In areas of contact with the affected meninges, there was marked vasculitis and perivasculitis, with accumulations of purulent exudate. Meningitis was observed throughout most of the affected cerebral hemisphere. Within the neurological tissue adjacent to the abscesses there were varying degrees of vasculitis, liquefaction necrosis, vascular proliferation, astrocytosis, neuronal necrosis and degeneration, and tissue edema. Special stains (GMS and PAS) demonstrated no mycotic agents.
Figure 3: Histological section of the cerebrum of a 2.5-month-old mixed-breed pig. Intracerebral abscesses (arrows) are poorly surrounded by connective tissue (hematoxylin-eosin, original magnification × 40). 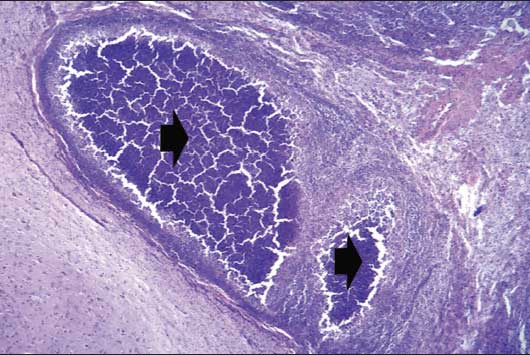 |
Bacteriological characteristics
Streptococcus suis was identified by biochemical evaluation, as described,1,3 from the swabs and brain sections. The bacterium was a gram-positive coccus that produced alpha hemolysis on sheep blood agar, reacted negatively to the V-P and NaCl assays, and produced acid in trehalose and salicin broths. Other biochemical characteristics included positive reactions with esculin hydrolase, arginine hydrolase, maltose, glucose, inulin, and lactose, but negative reactivity to sorbitol and catalase.
Molecular characterization
The desired partial 459 bp fragment of the capsular gene of S suis serotype 2 was amplified from the cultured bacteria submitted for PCR assay to the Veterinary Microbiology Diagnostic Laboratory, UFMS.
Discussion
The clinical signs observed in this case have been described in porcine streptococcal-induced meningitis.10,19 The pathological findings are manifestations of cerebral abscesses, while the bacteriological characteristics of the pathogen are consistent with those attributed to S suis.1,3 Further, PCR assay using DNA derived from the cultured bacteria amplified the 459 bp fragment of the capsular gene of S suis serotype 2; similar results have been described.17,18 Therefore, the absence of other infectious agents, as demonstrated by histochemical staining (PAS and GMS), suggests that S suis serotype 2 participated in the etiopathogenesis of the cerebral abscesses observed in this animal. To our knowledge, this case represents the first description of S suis-induced cerebral abscesses in swine without pathological manifestations of systemic disease. Microabscesses of the brain have been described in slaughtered pigs with extraneural demonstration of S suis infection.15 Abscesses in pigs are more frequently associated with S porcinus in the formation of jowl abscesses,3,10,16 during which multiple peripheral lymph nodes are affected. Abscesses were not observed within the lymph nodes of this pig. Additionally, purulent streptococcal meningitis or meningoencephalitis10,20 is more frequently attributed to the neurological manifestations observed in this pig. Therefore, we propose that these lesions be considered atypical manifestations of streptococcal meningoencephalitis.
In this case, there was histological manifestation of extensive purulent meningoencephalitis and well-encapsulated cerebral abscesses. Meningitis, meningoencephalitis, or both are common neurological manifestations of S suis.10,15,20 Meningitis with purulent vasculitis with extension of disease into the choroid plexus and spinal cord has been described in pigs experimentally infected with S suis.19 Although the pathogenesis of S suis meningitis has not been completely elucidated, it has been proposed that the bacterium can gain entry into the brain by destruction of the blood-brain-barrier.5,10 Further, the actions of the suilysin protein19 and other virulence factors5 are key elements to understand the mechanism of streptococcal meningoencephalitis.
The method of brain involvement in this case remains obscure, but active vascular dissemination from extraneural organs was not considered the source of infection, since pathological alterations suggestive of initial bacterial lesions were not observed in any tissue or system examined. Nevertheless, as a complete bacteriological evaluation was not performed (ie, bacteriological evaluation of samples from different organs), it is likely that the animal had recuperated from an extraneurological manifestation of purulent infection, since the onset of disease was observed at least 21 days prior to necropsy. Hence, it is reasonable to assume that the animal was bacteremic before being euthanized, with hematogenous dissemination to the brain terminating in bacterial sequestration at the meninges or neurological tissue21,22 and progressing to chronic abscess formation. The extensive nature of the meningitis associated with the close proximity to the right ear might suggest extension from a transient infection of otitis interna,22 but corresponding characteristic clinical manifestations were not related and typical gross lesions were not observed when the brain was being removed. Additionally, initial bacterial colonization within the nasal mucosa,5 with transient rhinitis and subsequent dissemination to the brain via the cribriform plate,22 cannot be discarded as a possible source of contamination. Therefore, a resolved extraneural lesion cannot be completely excluded as the source of contamination for the brain, since forms of direct extension to the brain were not observed.
Nevertheless, the brain lesions of this pig probably initiated at the meninges (acute meningitis) and progressed into the right cerebral hemisphere, resulting in multiple abscesses (chronic space-occupying lesions). Although extension of bacterial infection via the dura is uncommon, this results in localization of the abscess at the meninges,21 as occurred in this case. The involvement of the ependymal layer of the cerebral ventricle with the abscesses in this pig and of meningitis in pigs experimentally infected19 further demonstrates the progressive nature of S suis-induced meningoencephalitis. Therefore, we believe that these lesions should be considered atypical manifestations of S suis serotype 2 infection, which progressed from acute purulent meningitis to cerebral abscesses. The thickened fibrotic capsule of the abscesses closest to the meninges was additional evidence that the lesions were stepwise progressions, since fibrous encapsulation of abscesses within the brain is rudimentary unless the abscess is close to the meningeal surface, which is a source of collagenous tissue.21,22 This reflects the incapacity of the neurological parenchyma to synthesize adequate amounts of connective tissue, as was observed in abscesses located deep within the brain. It must be highlighted that this case is unusual, since the pig was not treated at the veterinary hospital due to the absence of neurological manifestations while the animal was observed for 2 days, and it is uncertain what therapeutic measures were administered at the farm.
Although cerebral lesions are frequent sequelae of either streptococcal endocarditis15 or arthritis,14 these conditions were not observed in this pig. Recently, cerebral microabscesses and granulomatous encephalitis were described in a study of slaughtered pigs with endocarditis-associated brain lesions.15 These histological alterations were not observed in this pig. Further, the distribution of brain lesions associated with left-side valvular endocarditis in pigs is focal and disseminated.15 The lesions of this pig were extensive, space-occupying, and asymmetric. Consequently, the morphology and distribution of the brain lesions observed in this case are different from those described in slaughtered pigs with brain-associated endocarditis.
Epidemiological studies performed in the geographical location of this farm have demonstrated that S suis serotype 2 is the most predominate serotype in clinically affected pigs.6-8 These data agree with the atypical finding of asymmetrical cerebral abscesses induced by S suis serotype 2 in this pig. Furthermore, S suis serotype 2 is most frequently associated with diseases of pigs worldwide.5
Implications
• Cerebral abscesses represent an unusual manifestation of streptococcal meningoencephalitis of swine.
• Diagnosis of cerebral abscesses should be based on characteristic gross and histopathological features and bacteriological culture.
• PCR targeting the capsular gene of S suis serotype 2 is an adequate diagnostic method to further characterize this pathogen.
Acknowledgements
This study was partially financed by the Pró-Reitoria de Pesquisa e Pós-Graduação, Universidade Norte do Paraná. The authors are grateful to Dr Geraldo Guerino Neto for the submission of this case for routine necropsy. We thank Dr Valéria Dutra, Universidade Federal de Mato Grosso, Cuiabá, MT, Brazil, for performing the molecular techniques used during this study. Dr S. A. Headley is a recipient of the National Council for Scientific and Technological Development (CNPq; Brazil) fellowship.
References
1. Higgins JM, Gottschalk M. An update on Streptococcus suis identification. J Vet Diagn Invest. 1990;2:249–252.
2. Staats JJ, Feder I, Okwumabua O, Chengappa MM. Streptococcus suis: past and present. Vet Res Commun. 1997;21:381–407.
3. Songer JG, Post KW. Veterinary Microbiology: Bacterial and Fungal Agents of Animal Disease. Saint Louis, Missouri: Elsevier/Saunders. 2005:43–53.
4. Higgins R, Gottschalk M, Boudreau M, Lebrun A, Henrichsen J. Description of six new capsular types (29–34) of Streptococcus suis. J Vet Diagn Invest. 1995;7:405–406.
5. Gottschalk M, Segura M. The pathogenesis of the meningitis caused by Streptococcus suis: the unresolved questions. Vet Microbiol. 2000;76:259–272.
6. Pagnani KJR, Castro AFP, Gottschalk M, Silveira WD, Nakazato G. Serotyping of Streptococcus suis strains isolated from pigs in the States of São Paulo, Minas Gerais and Paraná, Brazil. Pesquisa Veterinária Brasileira. 2002;22:1–5.
7. Martinez G, Castro AFP, Pagnani KJR, Nakazato G, Silveira WD, Gottschalk M. Clonal distribution of an atypical MRP, EF, and suilysin phenotype of virulent Streptococcus suis serotype 2 strains in Brazil. Can J Vet Res. 2003;67:52–55.
8. Del’Arco AE, Santos JL, Bevilacqua PD, Faria JE, Guimarães WV. Swine infection by Streptococcus suis: a retrospective study. Arquivo Brasileiro de Medicina Veterinária e Zootecnia. 2008;60:878–883.
*9. Gottschalk M. Porcine Streptococcus suis strains as potential sources of infections in humans: an underdiagnosed problem in North America. J Swine Heath Prod. 2004;12:197–199.
10. Higgins JM, Gottschalk M. Streptococcal diseases. In: Straw BE, Zimmerman JJ, D’Allaire S, Taylor DJ, eds. Diseases of Swine. 9th ed. Ames, Iowa: Blackwell Publishing; 2006:769–783.
11. Sanford SE. Gross and histopathological findings in unusual lesions caused by Streptococcus suis in pigs. I. Cardiac lesions. Can J Vet Res. 1987;51:481–485.
12. Jensen HE, Gyllensten J, Hofman C, Leifsson PS, Agerholm JS, Boye M, Bent A. Histologic and bacteriologic findings in valvular endocarditis of slaughter-age pigs. J Vet Diagn Invest. 2010;22:921–927.
13. Sanford SE. Gross and histopathological findings in unusual lesions caused by Streptococcus suis in pigs. II. Central nervous system lesions. Can J Vet Res. 1987;51:486–489.
14. Vasconcelos D, Middleton DM, Chirino-Trejo JM. Lesions caused by natural infection with Streptococcus suis type 9 in weaned pigs. J Vet Diagn Invest. 1994;6:335–341.
15. Karstrup CC, Jensen HE, Aalbaek B, Leifsson PS, Boye M, Agerholm JS. Endocarditis-associated brain lesions in slaughtered pigs. J Comp Path. 2011;144:289–295.
16. Katsumi M, Kataoka Y, Takahashi T, Kikuchi N, Hiramune T. Biochemical and serological examination of ß-hemolytic streptococci isolated from slaughtered pigs. J Vet Med Sci. 1998;60:129–131.
17. Marois C, Bougeard S, Gottschalk M, Kobisch M. Multiplex PCR assay for detection of Streptococcus suis species and serotypes 2 and 1/2 in tonsils of live and dead pigs. J Clin Microbiol. 2004;42:3169–3175.
18. De Faria ACS, da Silva MC, Oliveira Filho JX, de Oliveira JT, de Paula DAJ, Chitarra CS, Nakazato L, Dutra V. Prevalence of Streptococcus suis type 2 using the polimerase chain reaction in slaughtered pigs in the State of Mato Grosso, Brazil [in Portuguese]. Ciência Rural. 2010;40:130–134.
19. Zheng P, Zhao YX, Zhang AD, Kang C, Chen HC, Jin ML. Pathologic analysis of the brain from Streptococcus suis type 2 experimentally infected pigs. Vet Pathol. 2009;46:531–535.
20. Reams RY, Glickman LT, Harrington DD, Thacker HL, Bowersock TL. Streptococcus suis infection in swine: a retrospective study of 256 cases. Part II. Clinical signs, gross and microscopic lesions and coexisting microorganisms. J Vet Diagn Invest. 1994;6:326–334.
21. Summers BA, Cummings JF, de Lahunta A. Veterinary Neuropathology. Saint Louis, Missouri: Mosby. 1995:156–159.
22. Zachary JF. Nervous system. In: Zachary JF. McGavin MD, eds. Pathologic Basis of Veterinary Disease. 5th ed. Saint Louis, Missouri: Elsevier/Mosby. 2012:771–870.
* Non-referred reference.

